IO Biomarkers
IO Biomarkers
IO has entered the therapeutic mainstream, particularly due to recent developments within the immune checkpoint blockade.1 However, without any additional insight to guide patient selection, IO therapies response rates can vary by patient and response patterns can be unpredictable.1,2 As such, the development of predictive biomarkers has become a major focus of the field, as they could help to identify appropriate patients for IO therapy.1,2
IO Biomarkers Include Both Patient and Tumour Factors
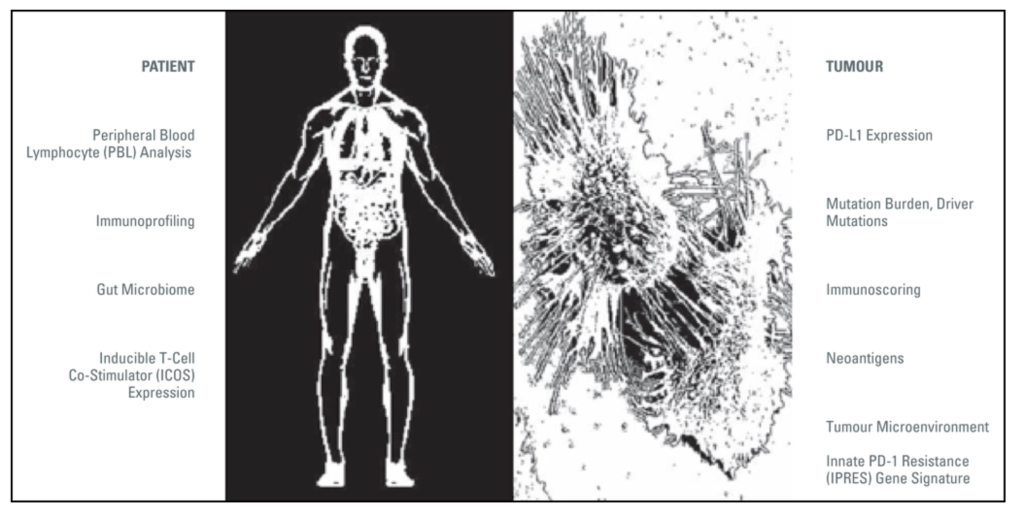
Adapted from Butterfield et al., 2017.1
The host immune system is only half of the equation in IO; the tumour and its surrounding microenvironment play important roles in the determination of immune tolerance, the metabolism of tumour cells and their propagation1. As such, IO biomarkers can include factors from both the patient and tumour2.
Select Examples of IO Biomarkers:1,2
PD-L1 Expression
The programmed cell death protein-1 (PD-1) pathway has been demonstrated to inhibit T-cell activation, a counter-regulatory pathway exploited by tumours to evade the immune system. Expression of PD-L1, one of the PD-1 ligands, has been described in a number of tumour types and has been found to be a positive biomarker for therapeutic response.
IL-6
Interleukin 6 (IL-6) is an important proinflammatory cytokine involved in innate immune response. Levels of serum IL-6 can inform on patients’ response to IL-2 therapy.
Mutation Burden
The mutational burden of tumours has been correlated with a higher probability of response to IO therapy, especially in those tumour types that are carcinogen-induced, such as melanoma and smoking-associated lung cancers. However, no specific genes have yet been associated with treatment response.
ICOS
Inducible T-cell costimulatory (ICOS) is a T-cell specific molecule that is expressed only T-cell activation. It is thought to play an important role in T-cell survival, proliferation, and the generation of memory T-cells. Studies suggest that the frequency of ICOS-positive CD4+ T-cells could be useful in determining patients’ response to anti-CTLA-4 therapy.
Peripheral Blood Biomarkers
A number of potential biomarkers are detectable in peripheral blood. For example, increased diversity and activation markers of peripheral blood lymphocytes (PBLs) have been associated with improved response to certain IO therapies, such as checkpoint inhibitors, while being a negative marker for treatments with others, including chemokine therapy. Other potential peripheral blood biomarkers include serum proteins, circulating tumour DNA, and other cellular factors.

IO BIOMARKERS PROVIDE INSIGHT FOR CLINICAL DECISION-MAKING. IT IS IMPORTANT TO ASSESS BIOMARKERS FOR EACH PATIENT TO HELP SELECT THE APPROPRIATE TREATMENT OPTION.2
PD-L1 = Programmed Death Ligand-1
References: 1. Butterfield, LH et al. Cancer Immunotherapy Principles and Practice. 2017. (Springer Publishing Company, Incorporated). 2. Spencer, KR et al. Biomarkers for Immunotherapy: Current Developments and Challenges. Am Soc Clin Oncol Educ Book. 2016;35:e493-503...
